Guest blog by Christina Horan

It was a December morning in 2017 when I found out I had breast cancer at age 34. Roughly a month and half earlier a lump had appeared in my left breast and instantly my stomach sank. I just had a feeling it wasn’t something benign like a cyst or fibroadenoma, likely because I knew 2 young women around my age who had been diagnosed with breast cancer in the previous few years.
I waited until my annual PCP appointment to have it checked. My doctor felt it and said, “I’m not sure what it is, but we don’t mess around. I’m sending you for a mammogram and ultrasound.” I am so incredibly lucky that I wasn’t brushed off as being “too young” or told it was, “probably just a cyst” as that is the case for many women my age.
My appointment was a week later. The night before I had gone Christmas tree shopping with my boyfriend, Patrick, who I had moved in with 6 months earlier. I remember thinking to myself as we went to bed, “this could be my last time going to sleep without breast cancer.” Thanksgiving had been a week prior, and the thought also crossed my mind that, “this could be my last Thanksgiving without breast cancer” as well. My gut is rarely wrong, and it was definitely trying to tell me something.
The next morning at my appointment I undressed and awkwardly tried to tie the robe they gave me to wear. (On a side note, it has been years and I still can’t tie that robe correctly!) I was given a mammogram and then I had an ultrasound. The ultrasound tech glided the wand over the area with the lump and was noticeably quiet. I tried to make conversation and ask questions about what she saw but she remained tight lipped. This was definitely a bad sign. The radiologist came in and said with a serious tone, “Listen, I’m not going to sugar coat this for you. What I see is very worrisome.” That was all I needed to hear. I burst into tears and asked for my mother who had accompanied me to the appointment. She came into the room and had tears in her eyes. I called Patrick and told him. I was scared and knew my world would change from this point forward.
Despite the blunt nature of the Radiologist, he ended up being a kind and caring man and made special arrangements so I could have a biopsy done that day. In addition, the nurse and ultrasound tech were also extremely kind and comforting. They both hugged me and told me I would be ok as I left. The nurse even gave me a magazine article on young women and breast cancer. I received the official diagnosis several days later: Stage 2 Invasive Ductal Carcinoma (IDC), Estrogen/Progesterone negative and HER2+. HER2 is a protein our bodies make, and mine was replicating abnormally at a rapid rate. What I had was an aggressive form of breast cancer and would need to have chemotherapy before anything else.
Next up was meeting my breast surgeon and then my oncologist a week later. He squeezed us in late in the day for an appointment, and by the time I saw him it was past 5pm. Still, he spent an hour or so talking my parents and Patrick through everything and the chemotherapy I would receive. He told me I would not have to receive the “Red Devil” aka AC (Adriamycin and cyclophosphamide) chemo, which can be tough on the heart. He also gave me the go ahead to go through egg freezing before starting treatment. That was a whole experience on another level, mixing up cocktails of drugs to inject myself with all while thinking, “I’m so not qualified to do this!” Overall, it was a success with 17 eggs being retrieved and frozen.
I breezed through the holiday season with a smile, not even telling anyone except immediate family until after our annual Christmas party that I had breast cancer. I mean, Santa was coming and I did not want people to focus on breast cancer and feel sorry for me. The best news was I even got engaged on New Years Eve! It was a happy but weirdly confusing and sad time.
I started 12 weeks of Taxol and Carboplatin chemotherapy in early January of 2018, along with targeted HER2 drugs Herceptin and Perjeta added every 3rd week. I developed a horrible rash after my 1st treatment that only started to heal after starting Doxycycline. Everything I ate tasted strange, and the only things I eventually found enjoyable were McDonalds cheeseburgers and macaroni and cheese. Ice cream was a lifesaver when I developed tongue and mouth sores. I would just dip my tongue in and let the cold provide relief. Due to the sores, I also started brushing my teeth with “toothettes,” which are basically a soft sponge on a stick. And of course there was the hair, eyebrow, and eyelash loss. I cried more on the day that I got my hair cut in a pixie than I did the day I actually shaved my head. I found myself some cute and comfortable hats because I did not like wearing my wig.
One thing I did not anticipate was losing my nose hair, which caused my nose to constantly drip wherever I was. I blew my nose at the grocery store once, and a man politely said, “allergies?” and I awkwardly started explaining how I had cancer which caused my nose hair to fall out and nose drip. I should’ve just nodded yes to the allergy question instead! Strangely enough I did not find the physical changes affected my mental health or mood too much. Thankfully I felt okay most of the time.
In May of 2018 I had a lumpectomy and a sentinel lymph node biopsy and in June I had a re-excision as they wanted a wider tissue margin because some DCIS (pre cancer cells that do not respond to chemotherapy) was found. My final pathology results were clear, with no active cancer remaining. The chemo had done its job. My oncologist told me my cancer was never coming back (a questionable thing, in my opinion, to tell a cancer patient). Most would be celebrating this result and telling anyone who would listen, but I felt like I would be jinxing myself. I just had a feeling it was too good to be true. And as you will find out later, it indeed was.
For now, life and treatment kept moving forward and radiation was up next. The job of radiation is to mop up any rogue cancer cells and thus decrease the chance of any recurrence. I found this part of the process to be very uneventful and I hardly had any discomfort. My left breast did become very tan, and my fiancée and I joked that it was like he was dating two different women. I also continued with Herceptin infusions as part of HER2+ protocol until March of 2019. I was officially “done” with treatment and had done everything recommended and offered, but my cancer story was far from over.
Patrick and I were married in May of 2019 and went on an amazing honeymoon to Italy and Croatia in June. I had my first post cancer mammogram in July. Some “punctate” calcifications were seen but they were deemed to be a result of surgery and radiation and didn’t look suspicious. I hated not having a completely normal result. However, I was cleared by my team to start trying to get pregnant in the fall and they recommended that I come back in 6 months for a follow up mammogram. Miraculously I got pregnant right away which was a shock as I was not sure it would be able to happen naturally at all. My little miracle guy Kellan was born in June 2020, right in the middle of the COVID pandemic. I never was able to get that recommended follow up mammogram as I was pregnant, but my team kept telling me they were not concerned.
I decided to try to breastfeed on my non affected side and my surgeon kept telling me they would wait until 6 months after I was done to do a mammogram, even on my cancer side that wasn’t producing anything. That just didn’t sit well with me based on my last abnormal mammogram and the fact that I had found out many women do still get mammograms while breastfeeding. I reached out to a trusted nurse at my cancer center and pleaded for a mammogram which she was able to make happen. My nerves kicked in and the tears flowed as I sang twinkle twinkle little star to my 6-month-old baby the night before my appointment.
Prior to admitting that there is something to be said for gut feelings (which I had before insisting on the mammogram) my surgeon made small talk with me before sharing that my mammogram in fact showed some abnormal calcifications that needed a biopsy. I was furious, and rightly so. My greatest fear had been realized. Had I ever even been cancer free this whole time? The radiologist performed the biopsy the next day which showed I had DCIS as well as a few invasive cells (still HER2+). The cancer was back. I called and demanded to speak with my oncologist, and angrily asked him why he told me I was cured. I believe his response was along the lines of trying to be positive. Looking back I regret making that call, because in the end it wasn’t his fault. I was just mad at the world.
Thankfully it seemed minimally invasive at only .04 cm. I got a second opinion, switched surgeons, and all doctors were in agreement on a double mastectomy as clearly the lumpectomy had not been enough. I was scheduled for surgery and immediate reconstruction. They would also potentially sample a few more lymph nodes, if possible, to make sure they were clear.
No one expected what happened next. I received my surgical pathology results online, of course, after 5pm when the surgeon’s office was closed, and got physically sick after reading the results. In between my biopsy and consultations with my doctors, (about 3 weeks’ time) a tumor the size of 11 cm had developed and was removed during surgery. In hindsight I was starting to show some classic signs of an aggressive form of cancer known as Inflammatory Breast Cancer (IBC), but the signs were misread even though I told my surgeon the symptoms I had. My surgeon thought I might have a hematoma from the biopsy and the previous treatment trauma. I also had a few bumps that started appearing which turned out to be skin metastasis. My surgeon even admitted to me that she thought about canceling my procedure, but the wheels were already in motion (not something a patient wants to hear from a surgeon who works at a world-renowned center).
IBC is always diagnosed as Stage 3 at minimum (and can very quickly progress to Stage 4) and it has a specific and aggressive treatment protocol that applies to most cases. First is chemotherapy, followed by a modified radical mastectomy and total axillary lymph node clearance, radiation, and then targeted therapy depending on pathology results from surgery and cancer subtype. I was petrified my cancer had spread as I had already gone out of this order. I had a skin sparing double mastectomy surgery with reconstruction and no lymph nodes removed. By the grace of God, I had a clear PET scan a week later. At that point I didn’t even care what was ahead of me, I just wanted to live.
A few days prior to my PET scan I started an aggressive chemotherapy regimen. This time I would not be spared from the “Red Devil”, and it was by far my toughest chemo experience. I ended up in the hospital twice with a neutropenic fever. I was exhausted and could barely lay on the couch to watch TV. That time was mostly a blur of Seinfeld episodes sandwiched between Old Navy commercials. Probably the worst part was being so disconnected from Kellan. I was too tired and sick to properly be his mother and therefore he became extremely attached to Patrick. Patrick is a fantastic father and husband, but it was hard on all of us.
Somehow I limped across the finish line and completed 16 sessions of chemotherapy. Next up was another surgery. This time, my surgeon removed the reconstruction and left me completely flat, taking as much skin as she could (IBC manifests itself in the breast skin). I was still eligible for reconstruction in the future but would have to use my own tissue and have a DIEP flap procedure. All remaining lymph nodes on my left side were taken and sent for testing. The pathology came back clear with no cancer found anywhere, but after what happened the last time I barely celebrated this result. I was suffering and much more depressed this time. I was still carrying some baby weight, I was completely bald with no lashes or brows, and had no chest to speak of, just ugly scars in its place. Most of all, I felt like an inadequate mother, as my son cried when alone in my presence because he wanted his dad.
You are told when you receive radiation that you can only receive it once in an area. Having it twice in the same area is virtually unheard of but was recommended in my case due to the 11 cm tumor and skin infiltration. It would be more aggressive and came with the risk of broken ribs and bone weakness (every woman I spoke with in my scenario of having radiation twice had in fact broken a rib afterwards at some point), increased future cancer risk, damage to the hearts and lungs, severe burns and the list went on. Eventually, kicking and screaming, I agreed to have it. I am not exaggerating when I say I hated every minute of it. I cried almost every treatment, I was burnt to a crisp, and it itched like crazy. Not only did I have no chest and barely any hair, but I also had a severely red, burned, and peeling chest now. It was probably my lowest point.
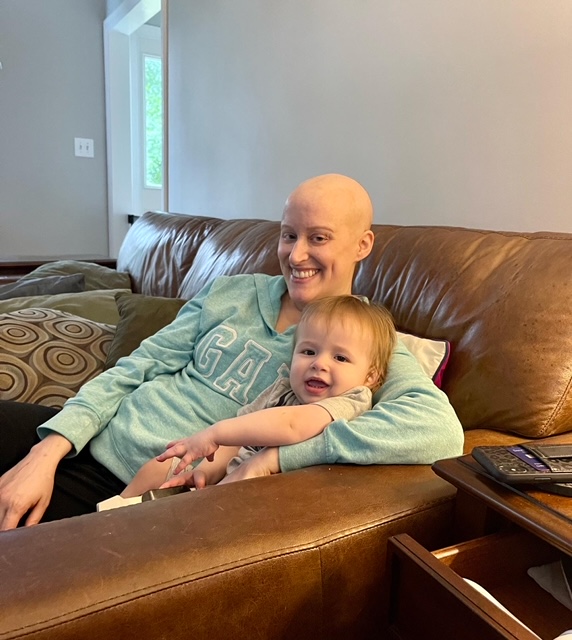
The last and final piece of my treatment puzzle was a drug named Kadcyla. It is called “smart” chemo, because the chemo part of the drug only targets the cancer cells and doesn’t destroy the healthy ones. During Kadcyla my hair continued to grow back, my radiation burns healed (though I will always have discolored skin and damage), I got in better shape, and we moved to a new house. After my 14 Kadcyla treatments I was able to have reconstructive surgery and I’m much happier with my body. My bond with my son is stronger than ever. He is the light of my life, along with my husband Patrick.
I feel like I’ve lived a few different lives now- cancer, wedding, pregnancy, pandemic, and cancer again. I would be lying if I said I don’t regularly think about my cancer coming back for a 3rd time, or worse spreading to other parts of my body. The thoughts haunt me every day and sometimes bring tears to my eyes. I don’t want to miss out on my son’s life. I hope someday I can tell him the story of how I battled cancer twice and that he will be proud of his mom. The biggest lesson I’ve learned is to always speak up, and fight for your care and answers if needed. You are your own best advocate and the only one with your best interest at heart.