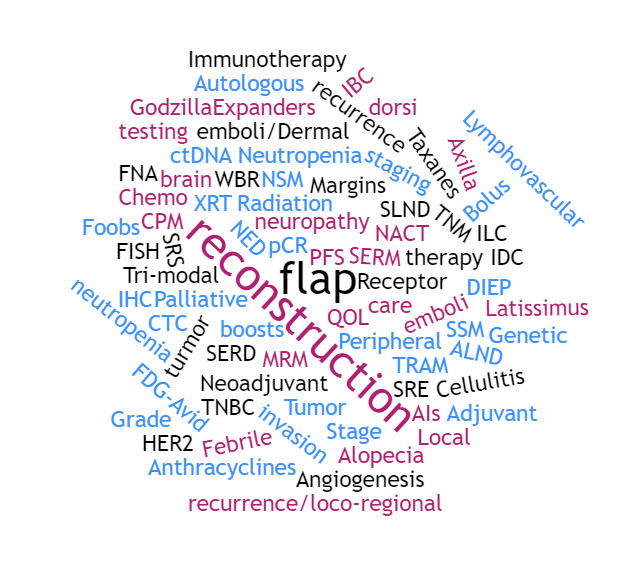
Navigating Breast Cancer- Terminology
A cancer diagnosis comes with terminology that could fill an encyclopedia. Newly diagnosed patients and their loved ones can have a hard time navigating the medical terms that come with their treatment plan. While this is by no means a complete list, here is a list of terms common to both Inflammatory Breast Cancer as well as other cancers.
Adjuvant
Therapies such as Herceptin or endocrine therapy that is given after surgical removal of all the known macroscopic disease in order to prevent recurrence.
AIs
Aromatase inhibitors (one type of anti-estrogen therapy used in ER+ breast cancers). They work by reducing estrogen synthesis by the aromatase enzyme in peripheral tissues such as fat and the adrenal glands.
ALND
Axillary lymph node dissection – the part of the surgery in which the surgeon takes out all the lymph nodes under your arm on the side of the invasive cancer to properly stage your cancer.
Alopecia
Alopecia means hair loss. Almost all IBC patients receiving chemotherapy experience this temporary side effect from anthracyclines and taxanes.
Angiogenesis
Angiogenesis is the process of tumor cells influencing the formation of new blood vessels to gain enough oxygen and nutrients to grow. This is a necessary step once the tumor has formed a clump of cells more than a few millimeters in size. IBC is known to induce these pathways at an early time point during progression.
Anthracyclines
A class of chemotherapy frequently used in breast cancer. These drugs work by damaging the DNA. Examples include Doxorubicin (Adriamycin), Epirubicin (Ellence) and Liposomal Doxorubicin (Doxil).
Autologous reconstruction
A general term for reconstructions using tissue from your own body. Examples include DIEP and TRAM flaps. If IBC patients desire reconstruction, delayed autologous methods are often the only options since implant procedures are difficult to do on radiated skin.
Axilla
Medical term for the armpit. There are lymph nodes there that are often the first sites of IBC spread beyond the breast, since the breast lymphatics drain to these nodes.
Bolus
A material that may be placed on the chest wall during radiation. The function of a bolus is to deposit more of the radiation dose in the skin versus deeper into the body. It can be made out of a plastic-type of material or other flexible material.
Cellulitis
A bacterial infection that can arise in the arms or elsewhere that can increase the risk for lymphedema. The symptoms include swelling, red skin, pain/tenderness, warmth. Importantly the redness can quickly spread and lead to sepsis and possible death if left untreated. Antibiotics are required either by IV or orally. Visit your doctor or emergency room if you think you have cellulitis.
Chemo brain
A constellation of long-term mental symptoms that arise in cancer survivors after chemotherapy, such as memory problems, difficulty concentrating, difficulty in multi-tasking and learning new skills. Although these symptoms are common, everyone is affected to a different degree.
CPM
Contralateral prophylactic mastectomy – this is when a woman with a tumor in one breast chooses to have the non-diseased breast removed to prevent recurrence or a second breast cancer.
CTC
Circulating tumor cells. CTCs are a research tool currently, useful in determining metastatic potential and perhaps molecular targets for therapy.
ctDNA
Circulating tumor DNA. This is cell-free DNA that is circulating in the blood that can be detected and sequenced to find mutations that can be targeted therapeutically. This is a promising research area, but not ready for prime-time in IBC care.
DIEP flap
DIEP stands for deep inferior epigastric perforator artery. It is a type of reconstruction using fat, skin, blood vessels from the lower abdomen, but no muscle tissue is used.
ER
Estrogen receptor is often shortened as ER. ER is one of 3 markers typically used on diagnostic and surgical specimens in breast cancer. ER binds to estrogen and mediates its growth effects in both normal and tumor cells.
Expanders
Immediate reconstruction methods with a plan to insert an implant later involves placement of an expander under the skin during the mastectomy. This is then filled with saline slowly to expand the skin sufficiently over several months prior to the next surgery to exchange expanders with the final implant. In IBC due to the amount of radiation to the skin, this method is not recommended due to high rates of failure and complications.
FDG-Avid
On a PET scan report, this term means the glucose tracer has been taken up at a level above background at that site. FDG-Avidity can mean tumor spread or be completely unrelated to cancer. Speak with your doctor about the interpretation of your report findings.
Febrile neutropenia
If low neutrophil count is accompanied with a fever (a sign of infection) then the symptom is referred to as febrile neutropenia.
FISH
Fluorescence In-Situ Hybridization, which is a method using a fluorescent probe to detect RNA molecules in tumor/normal tissues. By counting the signals in each cell you can tell whether a protein is overexpressed or not.
FNA
FNA stands for a fine needle aspiration. This is when a thin needle is used to do a small biopsy of a lymph node to determine whether there are any tumor cells present in the lymph node. If there are tumor cells in the lymph node, the node is counted as “positive”.
“Foobs”
A colloquial word for breast prosthesis. Some women who decide against reconstruction use prostheses to look more natural.
Genetic testing
If a woman has a significant family history of breast, ovarian and/or other cancers, she may be referred to a genetic counselor to consider testing for inherited mutations in cancer predisposition genes such as BRCA1 and BRCA2. Such results can be used for risk reduction and decision-making among the patient and their other family members, and also has potential therapeutic implications.
“Godzilla”
A term adopted by some patients for the drug Kadcyla (also known as T-DM1) due to its strong activity. Kadcyla is one of the first antibody-drug conjugates designed to be a targeted chemotherapy delivered to tumor cells overexpressing HER2.
Grade
The grade of a tumor tells you how aggressive it looks histologically. There are 3 potential grades – most IBCs are grade 2 or grade 3 (the most aggressive). This is distinct from stage.
Gy
When discussing radiation, Gy stands for Gray. It is a unit of measurement for the dose of radiation received.
HER2
Human epidermal growth factor 2, is the full name of the protein typically shortened as HER2. It Is frequently overexpressed in IBC, and a target for drugs such as Trastuzumab (Herceptin), or Pertuzumab (Perjeta). HER2 protein is on the membrane of tumor cells and signals to proliferation pathways to induce tumor growth and aggressiveness.
IBC
Inflammatory Breast Cancer. IBC is a clinical diagnosis of invasive breast cancer in the presence of the distinctive skin symptoms that can include redness, orange peel appearance (peau d’orange), ridging, pain in the breast, warmth, and swelling.
IDC
Invasive ductal carcinoma. This is the most common pathological diagnosis in IBC patients. It means that the tumor is invasive, and the tumor cells look like they came from the normal cells that line the ducts.
IHC
Immunohistochemistry – this is a method using antibodies to detect proteins in tumor sections. It is the standard method for determining ER, PR and HER2 status (although HER2 is also examined by FISH)
ILC
Invasive lobular carcinoma. This is a less common pathological diagnosis for IBC patients. It means that the tumor is invasive and looks like the cells in the milk-producing cells (lobules). Often lobular carcinomas have distant clinical behavior to ductal carcinomas.
Immunotherapy
Immunotherapy is a type of therapy being investigated in cancer that uses your body’s immune system to fight the cancer. Examples can include monoclonal antibodies, genetically engineered T cells and vaccines.
Latissimus dorsi flap reconstruction
This is a type of reconstruction that uses tissue from your upper back to construct the breast.
LE
LE stands for Lymphedema which is a swelling of the arm or even the upper body due to the inability to drain lymphatic fluid normally. This is an unfortunate side effect from lymph node removal and axillary radiation in a subset of breast cancer patients.
Local recurrence/loco-regional recurrence
When a recurrence develops either on the chest well near where the breast used to be, or in the axilla, the recurrence is termed as a local or loco-regional recurrence. This is in contrast to a distant recurrence which is a recurrence anywhere else (i.e. liver, lungs, brain, bones).
Lymphovascular invasion
This is a pathological term for the presence of tumor cells in lymphatic and blood vessels near the primary tumor. It is a sign of aggressiveness, since invasion of blood vessels is the first step in formation of distant metastasis.
Margins
After surgery, the goal is clean margins, ie no tumor on the edge of surgical specimen. If there is still tumor at the edge, then the margins are “dirty”. The goal of a curative surgery should always be clean margins, and if the surgeon does not feel this is likely to be possible, consultation with a multidisciplinary team is warranted to evaluate all the options for further treatment.
MRM
Modified Radical Mastectomy. This is the recommended form of surgery for IBC patients. It is sometimes also shortened online as “Mx”.
NED
No evidence of disease (ie on scans and physical exam)
Neoadjuvant (NACT)
Chemotherapy/systemic therapy that is given before surgery. NACT is the shortened form of the term ‘Neoadjuvant Chemotherapy’. In IBC this is the standard approach because at diagnosis the breast is inoperable.
Neutropenia
Low numbers of neutrophila (a type of white blood cell), which can be a frequent side effect from some types of chemotherapy (such as doxorubicin).
NSM
Nipple-sparing mastectomy. This is a type of mastectomy in which the breast tissue is removed, but the nipple is conserved, usually in preparation for a subsequent reconstruction. In IBC because of skin involvement, this is not recommended. A non-skin-sparing mastectomy is the recommended surgery for IBC patients.
OS
Overall survival
Palliative care
Palliative care is the management of cancer related symptoms to improve quality of life. It does not mean that the doctor has given up on you or that you are soon to die. Unlike hospice care, which is only at the end-of-life, palliative care can be given alongside treatments known to be effective against the cancer, and should be part of IBC management from diagnosis onwards. The word palliative is often used in metastatic patients for therapies that are not given with the goal of cure, but for improving the patient’s quality of life – for example decreasing pain from bone metastasis.
Peripheral neuropathy
A side effect from taxane chemotherapy that refers to numbness, tingling or shooting pain in the fingers or toes.
pCR
Pathological complete response – when drugs are studied in the neoadjuvant setting, this means there is no residual cancer cells (alive) in the surgery sample when the pathologist examines it. There are a few variations on how it is defined i.e. just in the breast or whether the lymph nodes must also be free of cancer.
PFS
Progression-free survival – in trials in metastatic patients, this is the time in which the patient lives without their disease becoming worse.
PR
Can be either Progesterone Receptor, or Partial Response (to a chemotherapy). Progesterone receptor is similar to ER, in that it is a hormone receptor that is measured on tumor cells to subtype the disease and decide upon treatment options.
QOL
Quality of life
Radiation boosts
During radiation to the chest wall, there will be some sessions near the end that are focused on specific areas (such as the area around the scar line). This is done to make sure any
Receptor
A protein that is located on the surface of a cell that binds to a hormone or growth factor. Some specific examples of relevance in IBC include the Estrogen Receptor (ER) and HER2.
SERM
Selective estrogen-receptor modulators. These are a type of endocrine therapy used in ER or PR positive breast cancer patients to reduce recurrence. Examples of SERMs that are used clinically include tamoxifen and raloxifene.
SERD
Selective estrogen receptor down-regulators. This is a type of endocrine therapy that works via degrading the estrogen receptor, therefore limiting the effects of estrogen. Examples of these drugs include Fulvestrant and ARN-810.
SSM
Skin-sparing mastectomy. This is a type of mastectomy in which some skin is not removed to make future reconstruction more straightforward. This is not recommended for IBC patients due to baseline skin involvement.
SLND
Sentinel lymph node dissection – This is not a recommended procedure for IBC patients, but is sometimes done at the time of surgery in other early breast cancers in which a blue and radioactive dye is injected into the breast and allowed to drain into the armpit (axilla). The nodes that are blue and/or radioactive are called the sentinel nodes and are the first lymph nodes that would be likely to harbor metastases if the cancer has developed that ability.
SRE
Skeletal-related events – in patients with bone metastases, one way of measuring the effectiveness of bone targeted agents (such as bisphosphonates) is to measure the time till a fracture or other serious event involving the bone like spinal cord compression. It can also relate to the time when radiation (or sometimes surgery) is necessary for pain relief.
SRS
Stereotactic radiosurgery. This is a focused type of radiation, used sometimes for brain or bone metastases. It can also be called Gamma Knife or Cyberknife.
Stage
The stage of a cancer means how far it has spread beyond the primary site. The earliest stage of IBC is IIIB, which means the tumor may have invaded the axillary nodes, but no distant organs. Stage IV means distant metastatic spread at diagnosis.
Taxanes
A class of chemotherapy that is frequently used in IBC. These drugs work via interfering with processes important in cell division. Examples include Paclitaxel (Taxol) and Docetaxel (Taxotere).
TNBC
Triple negative breast cancer (i.e. ER negative, PR negative and HER2 negative/not overexpressed). Sometimes this is also abbreviated TN-IBC for triple-negative IBC patients.
TNM staging
This is the usual method in which tumors are staged. T takes into account tumor size; N takes into account the number and location of positive lymph nodes, and M tells you whether you have distant metastases or not. By definition IBC patients are T4d. Most are N1-N3 due to lymph node involvement. If diagnosed with stage 4 disease (ie distant metastases) then M1 is the designation.
TRAM flap
A TRAM flao (transverse rectus abdominus muscle) reconstruction is a type of breast construction using tissue from your lower abdomen, including the rectus abdominus muscle.
Tri-modal therapy
This refers to the overall plan for IBC treatment involving all 3 modalities of cancer therapy – chemotherapy, surgery and radiation.
Tumor emboli/Dermal tumor emboli
One of the histological findings that is more common in IBC is the presence of nests of tumor cells in the deeper layer of the skin (the dermis).
WBR
Whole brain radiation
XRT
External-beam radiation, which is the usual kind for chest wall or whole breast radiation. The radiation beams are generated in a linear accelerator, i.e. outside the body.
The TNM Staging System
The TNM system is the most widely used cancer staging system. Most hospitals and medical centers use the TNM system as their main method for cancer reporting. You are likely to see the cancer described by this staging system in the pathology report, unless the have a cancer for which a different staging system is used. Examples of cancers with different staging systems include brain and spinal cord tumors and blood cancers.
In the TNM system:
- The T refers to the size and extent of the main tumor. The main tumor is usually called the primary tumor.
- The N refers to the number of nearby lymph nodes that have cancer.
- The M refers to whether the cancer has metastasized. This means that the cancer has spread from the primary tumor to other parts of the body.
When your cancer is described by the TNM system, there will be numbers after each letter that give more details about the cancer—for example, T1N0MX or T3N1M0. The following explains what the letters and numbers mean:
Primary tumor (T)
TX: Main tumor cannot be measured.
T0: Main tumor cannot be found.
T1, T2, T3, T4: Refers to the size and/or extent of the main tumor. The higher the number after the T, the larger the tumor or the more it has grown into nearby tissues. T’s may be further divided to provide more detail, such as T3a and T3b.
Regional lymph nodes (N)
NX: Cancer in nearby lymph nodes cannot be measured.
N0: There is no cancer in nearby lymph nodes.
N1, N2, N3: Refers to the number and location of lymph nodes that contain cancer. The higher the number after the N, the more lymph nodes that contain cancer.
Distant metastasis (M)
MX: Metastasis cannot be measured.
M0: Cancer has not spread to other parts of the body.
M1: Cancer has spread to other parts of the body.
ER and PR status are important in deciding upon whether endocrine therapy is needed after chemotherapy, surgery and radiation. If even 1% of tumor cells express ER or PR (also known as HR positive/HR+ tumors), some type of endocrine therapy would be recommended to decrease risk of recurrence. HER2 is particularly important to know before beginning treatment since the chemotherapy protocol is designed with this in mind. HER2 positive tumors receive HER2 targeted therapy along with chemotherapy. The current standard in the US for neoadjuvant treatment for HER2+ tumors includes Herceptin, Perjeta (Pertuzumab) and a taxane. There are a few options for the other drugs used. HER2 negative tumors do not receive Herceptin or Perjeta since the target of these drugs are not present at high levels. In terms of chemotherapy choices for HR+ or TN (triple negative) tumors, a number of cocktails may be used and these are usually selected based on the treating medical oncologist’s preference.
If you are unsure of what the abbreviations mean in your diagnosis, and feel your medical team has not adequately explained it to you, be sure to ask. We have spoken to some patients who have felt uncomfortable asking because they worry about offending their doctor. When you are the patient, your best advocate is yourself. It’s your health at stake, and you deserve to understand everything surrounding your care. Ask, ask more, and ask again. You have the right to expect thorough explanations.
Resources:
TheIBCNetwork.org
Cancer.net
Cancer.org